Story by Connor Danielowski / February 19, 2026
Chronic Care Management (CCM) is no longer a differentiator on its own. Most primary care and specialty clinics know CCM exists, and many have implemented it in some form.
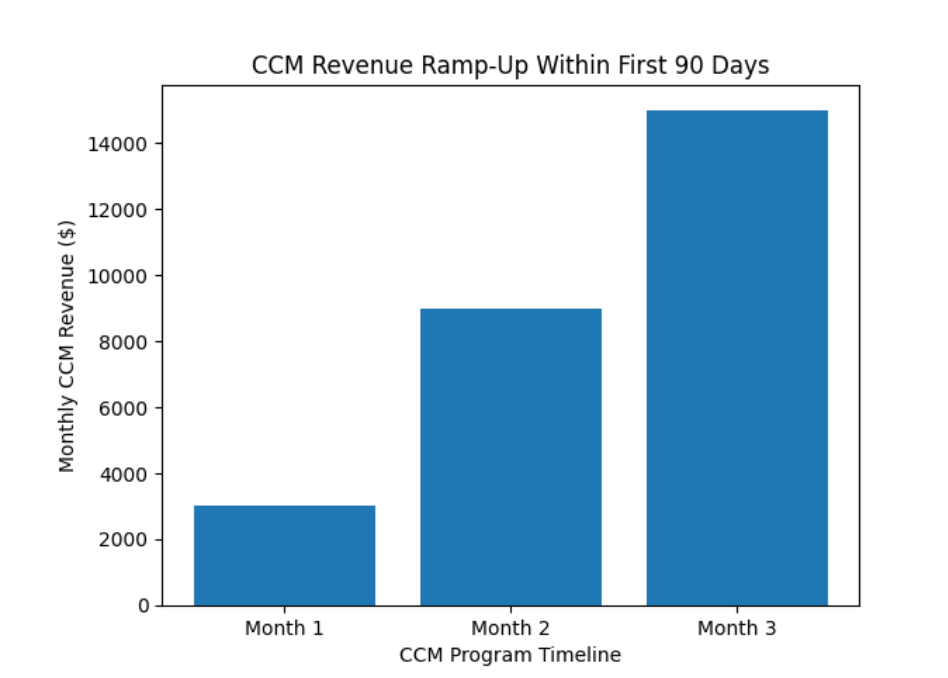
Yet revenue outcomes vary wildly.
Some clinics generate modest CCM revenue that barely moves the needle. Others—often serving similar patient populations—double or even triple CCM revenue per provider.
The difference is not patient demographics. It’s execution.
By benchmarking high-performing clinics against average performers, clear patterns emerge that explain why some organizations dramatically outperform their peers.

Across comparable practices, CCM performance often falls into two tiers:
Average-performing clinics
Top-performing clinics
The result is often 2x monthly CCM revenue, without seeing more patients or extending office hours.
High-performing clinics prioritize systematic patient enrollment, not passive opt-in.
Key differences:
Average clinics wait for patients to ask questions. Top clinics assume eligibility and guide patients through consent efficiently.
Benchmark insight: Clinics enrolling over half of eligible patients consistently outperform peers by wide margins.
CCM reimbursement depends on documented care coordination time. Top clinics ensure this happens every month, for every enrolled patient.
They succeed because:
Underperforming clinics often miss billable minutes simply because no one “owned” the process.
Benchmark insight: High performers don’t work more, they document better.
Clinics that double CCM revenue treat it like a service line, not an afterthought.
Leading clinics:
By contrast, average clinics spread CCM responsibilities across already-busy teams, leading to inconsistency.
Benchmark insight: Clear ownership drives accountability, and accountability drives revenue.
Top clinics don’t necessarily deliver “more” care—they deliver organized care.
They use:
This allows care teams to support more patients without burnout.
Average clinics often rely on reactive communication, which feels busy but produces less billable output.
Benchmark insight: Structure scales; chaos does not.

High-performing clinics understand that CCM is monthly recurring revenue, similar to a subscription model.
They plan around it:
Average clinics see CCM as “nice to have” income. Leaders see it as predictable financial infrastructure.
The patient population doesn’t change. The process does.
As healthcare shifts toward value-based models, CCM performance is becoming a competitive advantage.
Clinics that underperform:
Clinics that lead:
Clinics that double their CCM revenue are not doing anything exotic. They enroll patients intentionally, document consistently, assign ownership, and treat CCM like the revenue stream it is.
Benchmarking reveals a simple truth: CCM success is operational, not clinical.
For practices willing to refine their workflows, the gap between average and top-performing clinics is entirely bridgeable.

