Story by Connor Danielowski / January 12, 2026

Most clinics are familiar with Chronic Care Management (CCM) and Remote Patient Monitoring (RPM) as separate programs. What’s often overlooked is how powerful these services become when implemented together.
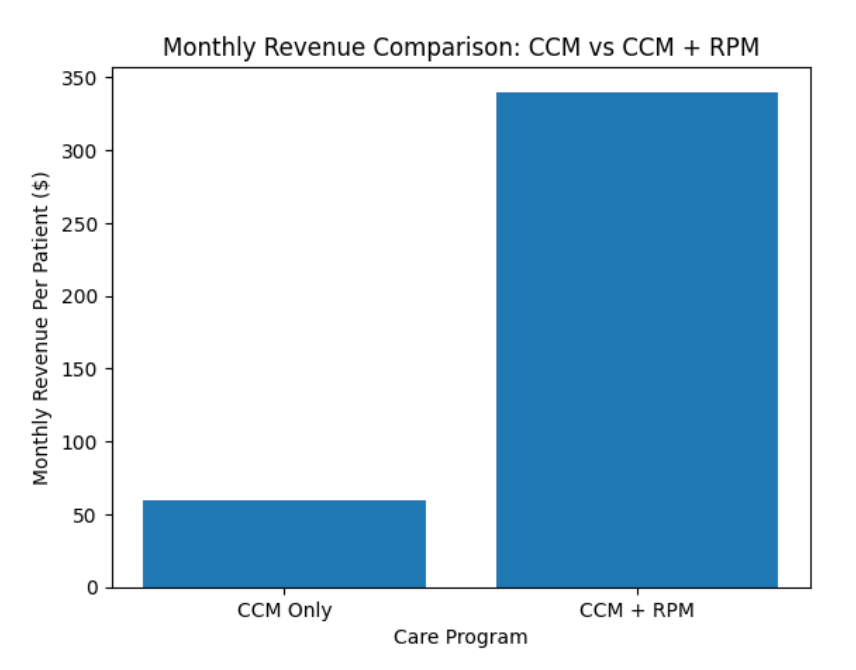
When CCM and RPM are properly aligned, clinics unlock what many don’t realize exists: a billing multiplier that significantly increases monthly revenue per patient, without adding in-office visits or increasing provider workload.
In many practices, this combined model can generate up to $349.05 per patient per month, while simultaneously improving patient engagement, outcomes, and care continuity.
Here’s how it works, and why clinics that combine CCM + RPM outperform those that run them in isolation.
CCM and RPM were designed to complement each other under Medicare’s care management framework.
Together, they create a closed-loop care model:
This alignment doesn’t just improve care—it strengthens documentation, supports compliance, and maximizes allowable reimbursement.
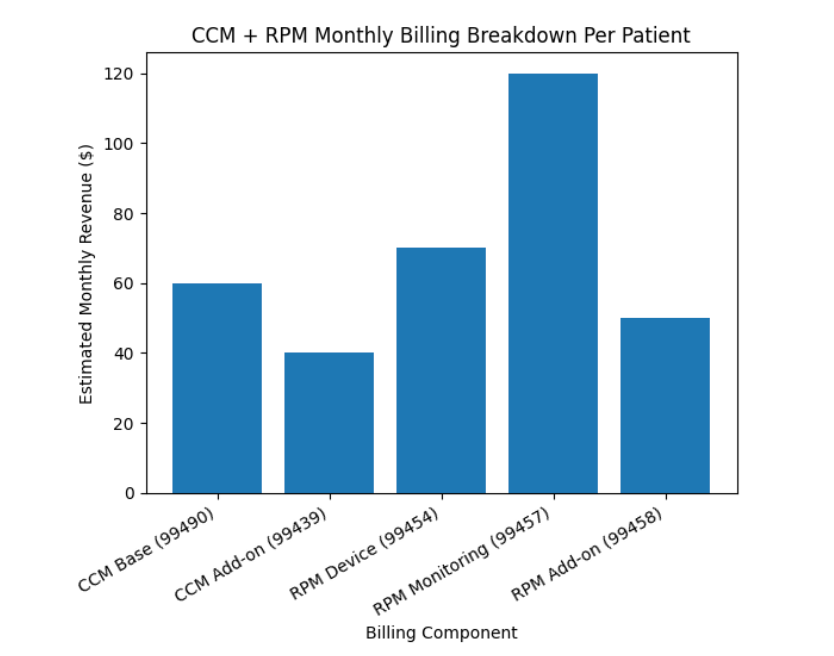
The billing multiplier comes from stacking compliant, CMS-approved CPT codes across CCM and RPM services.
Remote Patient Monitoring (RPM)
When these services are delivered and documented correctly, the combined reimbursement can reach:
Up to $349.05 per patient per month
Actual reimbursement varies based on payer mix, time thresholds, and patient eligibility.
Read our blog on “Money Left on the Table”: How to Capture Untapped Medicare Revenue Through CCM (CPT Codes 99490 & 99439)

The opportunity exists, but many clinics fall short due to operational friction.
Common issues include:
The result? Clinics run both programs but only capture a fraction of the revenue they’re eligible for.
Clinics that successfully capture the billing multiplier typically share three traits:
CCM and RPM workflows are coordinated, not separate. RPM alerts trigger CCM outreach, documentation, and follow-up.
Time spent across both services is tracked cleanly, compliantly, and in real time.
Patients understand why they’re being monitored and how care teams are supporting them—leading to higher adherence and longer enrollment duration.
This structure doesn’t increase provider workload. In most cases, it reduces administrative strain by creating clarity and consistency.
The billing multiplier isn’t just financial, it reflects better care delivery.
Patients enrolled in both CCM and RPM often experience:
From a value-based care perspective, this model aligns incentives across providers, patients, and payers.
For clinics focused on long-term sustainability, combining CCM + RPM creates:
Most importantly, it allows clinics to serve high-risk patients more effectively—without sacrificing operational efficiency.
The $349.05 per patient per month isn’t a new program or loophole—it’s the result of fully leveraging CMS-approved care models the way they were intended to work together.
Clinics that recognize and implement this combined approach don’t just increase revenue. They build more resilient, patient-centered care systems that scale with confidence.

GET IN TOUCH