Story by Connor Danielowski / December 1, 2025

Story by Connor Danielowski / December 2025
Every provider knows the pattern: a patient appears stable during their appointment, leaves with a detailed care plan… and then reappears weeks later in the emergency room.
What happened?
The truth is simple:
The most dangerous part of chronic disease management is the time between appointments-not the visit itself.
Quick Answer:
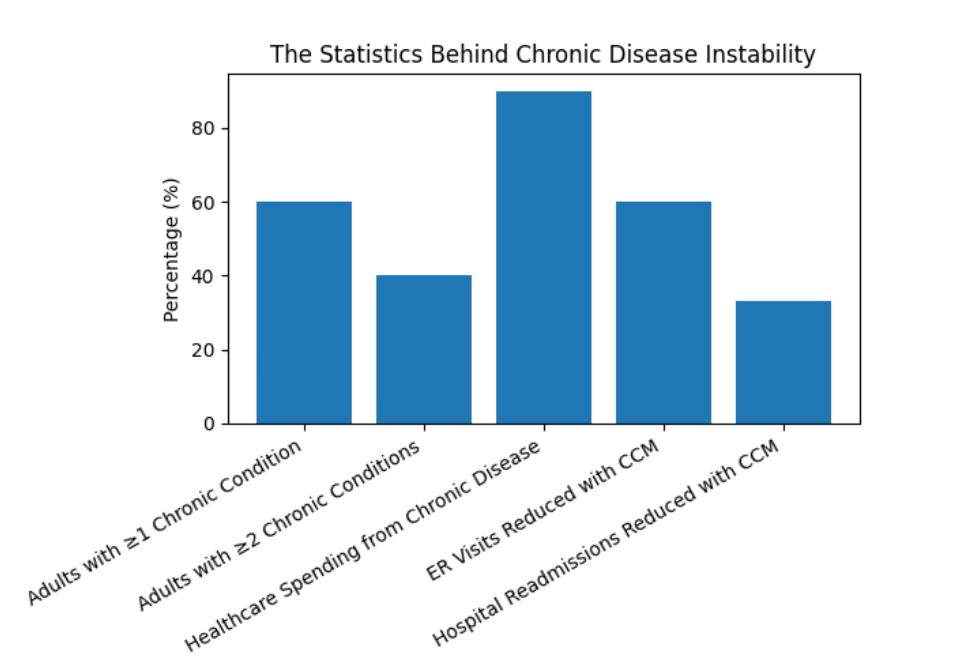
Chronic Care Management reduces emergency room visits by 60% and readmissions by 33% because it fills the care gap between office visits with proactive monitoring, medication support, symptom tracking, and consistent patient communication. Patients don’t slip through the cracks-because someone is watching.

Patients managing chronic conditions-diabetes, CHF, COPD, hypertension, CKD, and others-are expected to self-manage complex care instructions day after day. They juggle:
Yet there is no clinical touchpoint to help them navigate these challenges between visits unless a crisis forces them to seek emergency care.
This is where Chronic Care Management becomes transformative.

Medicare created CCM to solve a very specific problem:
Patients were crashing in the gaps between appointments.
Traditional appointment schedules cannot provide the ongoing guidance high-risk patients need. CCM bridges that gap with structured monthly support that includes:
This shift moves care from reactive crisis management to proactive condition stabilization.

Even highly engaged patients hit barriers. Consider how quickly things can unravel:
Without regular check-ins, adherence falls apart and acute episodes follow.
A simple reminder or transportation arrangement could prevent a hospitalization.
Patients often don’t recognize warning signs-or assume symptoms will “go away.”
Each breakdown leads to one of two outcomes:
an ER visit or a readmission.
CCM eliminates these breakdowns by keeping eyes on the patient every single month.
The data is crystal clear:
Patients without between-visit support get worse.
Patients with structured monthly touchpoints get better.
Emergency room reductions occur because CCM coordinators intervene early-long before issues escalate into emergencies.
Monthly check-ins catch red-flag symptoms before they trigger an ER trip.
Coordinators correct issues like missed doses, incorrect timing, or conflicting medications.
Instead of waiting until symptoms become unbearable, patients receive timely office-based intervention.
Ensuring patients complete follow-ups and labs keeps their care plans on track.
Result:
Patients stabilize, not spiral.

The 30-day post-discharge window is the most high-risk period.
CCM directly impacts this stage by providing:
A coordinator checks in, reviews discharge instructions, and ensures patients have their medications.
Patients are coached to report concerning signs instead of waiting until it’s too late.
Social determinants-transportation, food insecurity, cost of medications-are addressed proactively.
Patients understand what to do, when to do it, and who to call.
These simple, structured steps prevent unnecessary rehospitalizations.
Patients respond differently when outreach comes from their doctor’s office-not a random call center.
When CCM coordinators introduce themselves under the practice name, trust increases.
This leads to:
Trust alone changes clinical outcomes.
Effective CCM programs evaluate and address social determinants of health that directly impact stability:
These non-clinical barriers often matter more than the clinical diagnosis itself.
CCM identifies and addresses them-one by one.

It isn’t that providers don’t want to deliver CCM; it’s that they don’t have the time.
Common challenges:
This is why many practices choose a specialized CCM partner-they can achieve consistent, measurable outcomes without increasing internal workload.
Effective programs track:
A well-run CCM program improves every metric simultaneously.
When patients feel supported and monitored between visits, outcomes change:
The healthcare system improves not because care becomes more complex-but because it becomes more consistent.
If your organization is still relying solely on appointments to manage high-risk patients, you’re leaving outcomes-and revenue-on the table.
CCM makes proactive care possible.
We make CCM simple.
Want to see what outcomes your practice could generate with a fully managed CCM program? We can analyze your patient population and show the projected reductions in ER visits, readmissions, and overall cost.
