Story by Connor Danielowski / February 16, 2026


For decades, most medical practices have relied on a simple equation: no visit, no revenue. Patient volume goes up, revenue follows. Visits slow down, cash flow tightens.
But healthcare delivery has changed—and so has reimbursement.
Chronic Care Management (CCM) allows practices to generate predictable, recurring revenue every month, even when patients are not physically coming into the office. Instead of tying financial performance to visit schedules alone, CCM creates a steady billing stream built around ongoing care.
This shift is especially important for practices managing Medicare patients with multiple chronic conditions, where consistent engagement matters just as much as in-person appointments.

Traditional fee-for-service models create unavoidable revenue volatility:
Even high-performing practices feel this strain. When revenue depends almost entirely on office visits, financial stability becomes unpredictable.
At the same time, providers are still delivering care between visits—answering calls, coordinating medications, updating care plans, and following up on patient needs—often without reimbursement.
Chronic Care Management reimburses practices for non-face-to-face care delivered throughout the month. Instead of billing only when a patient is seen, CCM recognizes the ongoing work required to manage patients with chronic conditions between office visits.
To qualify, patients must:
Once enrolled, practices can bill CCM every month, as long as care coordination requirements are met.
This creates a revenue model that is:

With CCM in place, practices earn reimbursement whether or not the patient comes into the office that month.
That means:
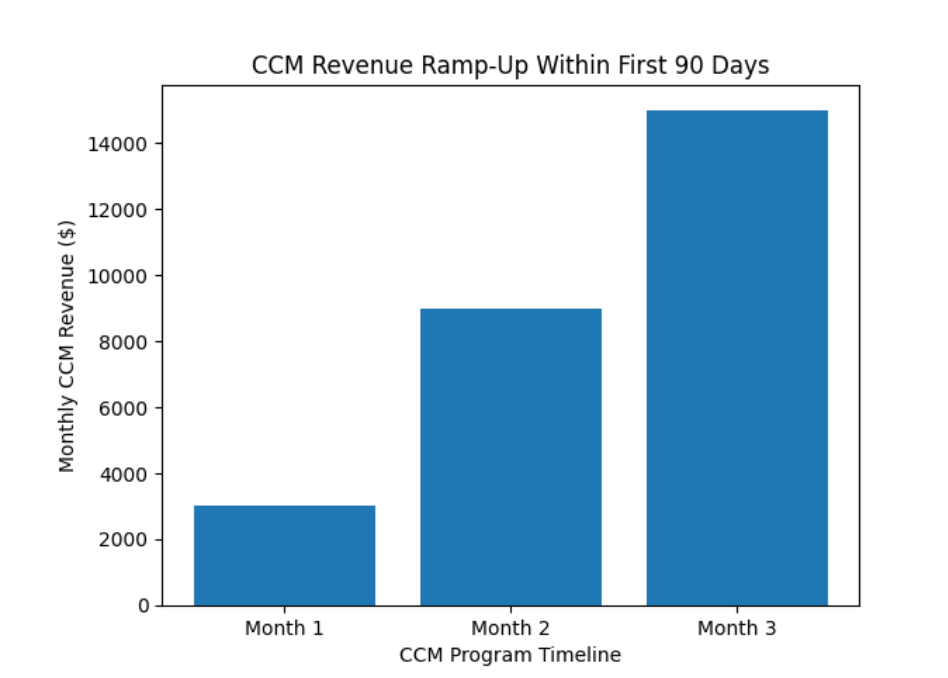
Instead of spikes and dips tied to the appointment calendar, CCM smooths cash flow into a monthly baseline of predictable income.
For many practices, this becomes the financial foundation that stabilizes operations.
Between office visits, CCM covers activities such as:
These tasks directly improve outcomes—and now, they also generate revenue.
Rather than being seen as an overhead or administrative burden, care coordination becomes a reimbursable service line.
Consistent monthly revenue unlocks operational advantages that visit-based billing cannot:
For growing practices, CCM revenue often funds:

CCM is not a replacement for in-person care. It works alongside traditional visits to create a more complete financial and clinical model.
Office visits still generate revenue. CCM simply fills the gaps between them—ensuring care continuity and income continuity at the same time.
When visits slow down, CCM keeps revenue moving.
Visit-based billing treats care as a series of disconnected moments. CCM recognizes what providers already know: chronic care happens every day, not just on appointment dates.
By shifting from episodic billing to ongoing monthly reimbursement, practices gain:
Chronic Care Management allows practices to move beyond the limitations of visit-based billing. Instead of tying revenue solely to office traffic, CCM creates a consistent, monthly cash flow driven by real patient care delivered between visits.
For practices looking to stabilize revenue, improve patient outcomes, and build a more sustainable financial model, CCM is no longer optional—it’s foundational.

