Story by Connor Danielowski / January 6, 2026

Launching a Chronic Care Management (CCM) program often comes with one big question:
How long before this actually generates revenue?

For most clinics, the answer is clear and consistent: within 30 days of going live.
When CCM is implemented correctly, with compliant workflows, patient engagement, and operational support, clinics typically begin seeing meaningful, recurring revenue within the first three months. This period is known as the CCM ramp-up, and understanding what happens during each phase helps set accurate expectations and ensures long-term success.
Below is a realistic look at how clinics move from launch to revenue within a single quarter.

The first month focuses on building the foundation. While revenue is not the primary outcome during this phase, it is where future reimbursement is unlocked.
Most clinics start by enrolling 20–40% of their eligible population in the first month. This is intentional, rushing enrollment often leads to documentation gaps or patient confusion.
Key takeaway: Month 1 sets up predictable revenue, even if cash flow hasn’t fully started yet.
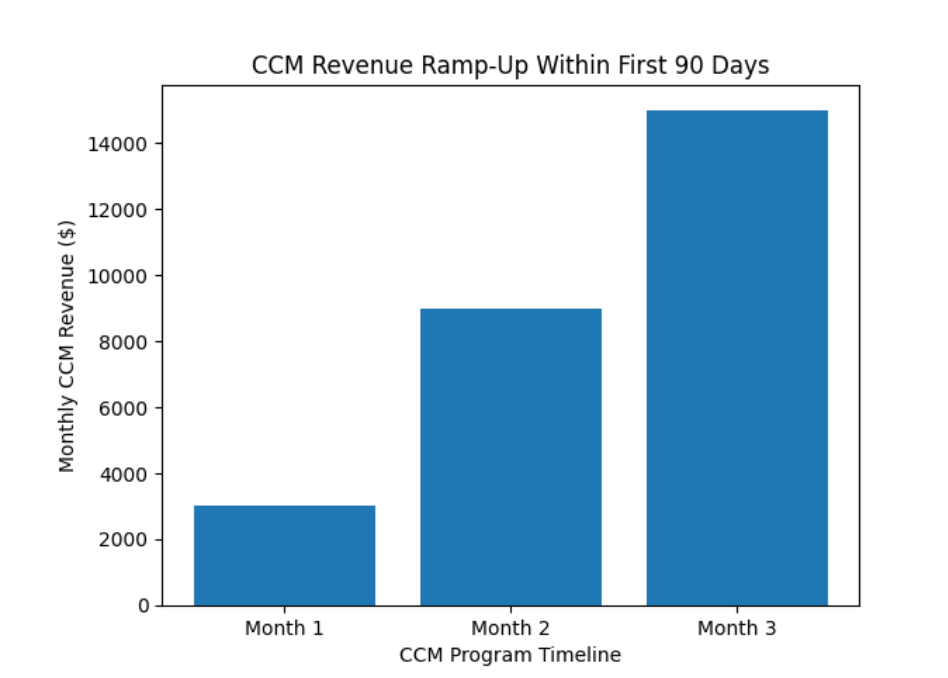
Month 2 is where CCM shifts from setup to execution.
Patients are now actively receiving:
Care teams are consistently documenting time spent, which is critical for billing compliance.
For a clinic with 100 enrolled CCM patients:
Key takeaway: Month 2 is typically the first month clinics feel the financial impact of CCM.
Build a Model of Recurring Revenue Growth with Chronic Care Management

By Month 3, CCM becomes operationally routine, and financially reliable.
At this point:
Clinics often expand enrollment further once they see consistent results.
Using conservative estimates:
Key takeaway: By the end of Month 3, CCM is no longer an experiment, it’s a dependable revenue stream.

CCM ramps faster than many clinical programs because:
When paired with experienced CCM partners, clinics avoid the most common delays:
If your clinic has not yet implemented CCM, it’s important to understand that waiting also has a cost.
Every month without CCM means:
Clinics that launch CCM today are often surprised by how quickly it integrates into daily operations, and how fast it begins contributing financially.
The 3-month ramp-up is not a barrier, it’s a runway.
Within one quarter, clinics typically move from planning to predictable, compliant revenue while simultaneously improving patient engagement and care coordination.
With the right infrastructure and support, CCM becomes one of the most sustainable programs a clinic can offer, clinically and financially.
