Story by Connor Danielowski / January 23, 2026
As we move into 2026, the conversation around Medicare reimbursement for Chronic Care Management (CCM) and Remote Patient Monitoring (RPM) shouldn’t be about whether these programs matter—it should be about why you haven’t fully committed yet.
Here’s the reality: patients with multiple chronic conditions are driving your highest costs and consuming the most resources. CCM and RPM are designed specifically to address this—by paying you for the care that’s already happening (or should be happening) between visits. The 2026 updates include meaningful rate increases that make this an ideal inflection point to get serious about these programs.
Medicare has increased reimbursement rates across both CCM and RPM for 2026. Here’s what that looks like:
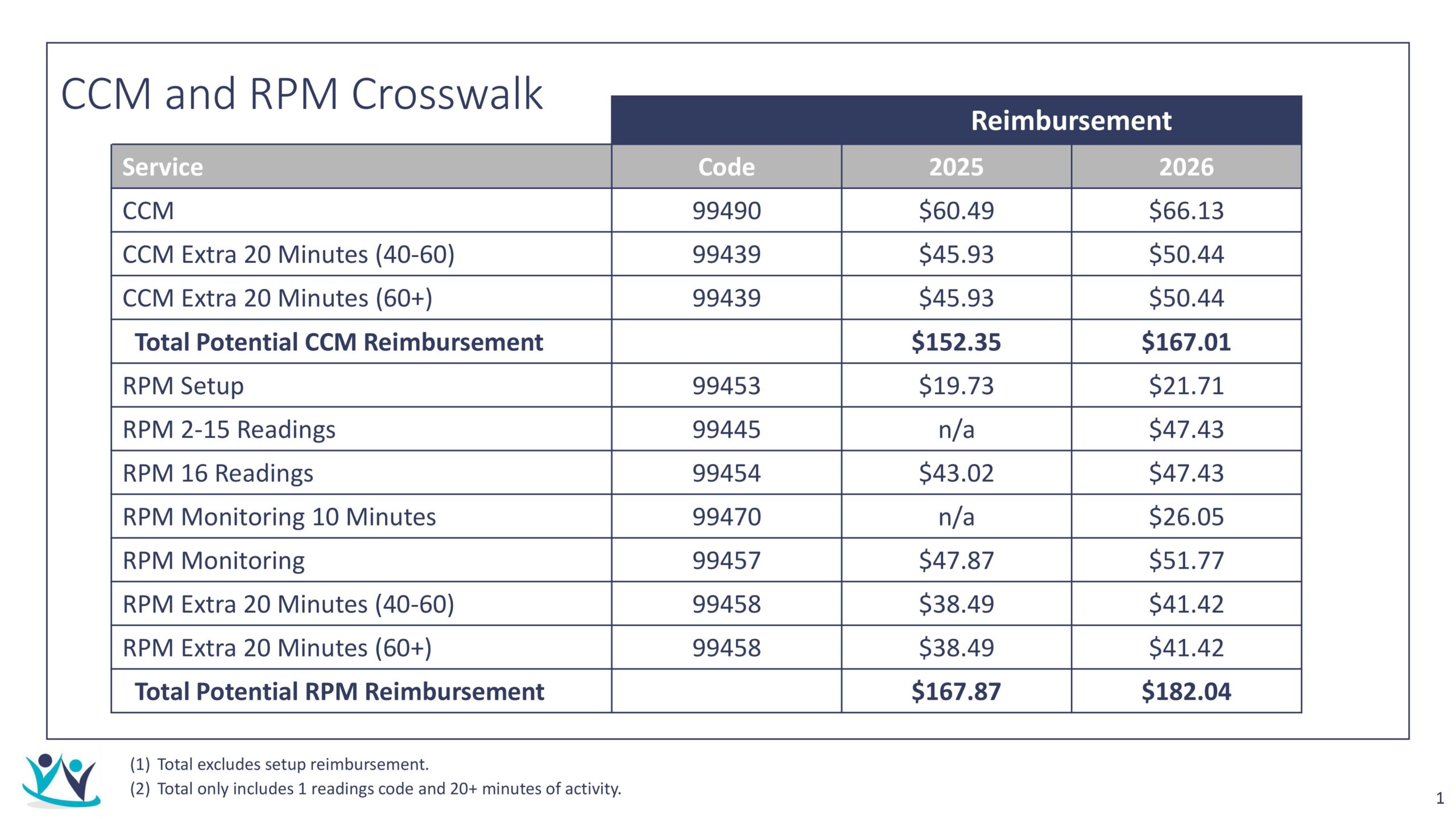
The increases aren’t dramatic, but they’re deliberate. CMS is signaling continued commitment to proactive, longitudinal care. For practices that have been on the fence, this is a natural moment to reassess.
CCM reimburses you for structured, non-face-to-face care coordination. The kind of work your staff is probably already doing—calling patients, adjusting medications, coordinating with specialists, following up on labs.
The difference? When it’s formalized as CCM, you get paid for it. When it’s not, you’re absorbing the cost.
Higher reimbursement tiers exist for a reason: complex patients require more time, more follow-up, more intervention. If you’re managing unstable diabetics, heart failure patients, or anyone juggling multiple specialists, you already know this. CCM is built to reflect that reality.
But here’s the catch: you only capture the revenue if you meet the time thresholds and document the work. Most practices that “try” CCM and fail don’t have a reimbursement problem—they have an execution problem.
RPM isn’t about handing out blood pressure cuffs and hoping for the best. It’s about using objective, real-time data to drive better care decisions.
The reimbursement structure makes this clear: you get paid for device setup, for data transmission, and for clinical time spent reviewing and acting on that data. If you’re not using the information to adjust care plans, reach out to patients, or escalate when needed, you’re missing the point.
The practices seeing real results with RPM aren’t treating it as a separate initiative. They’ve integrated it into their workflows. The data informs the care plan. The care plan drives the monitoring. It’s a loop, not a one-off project.
You can run CCM or RPM independently, but there’s real value in combining them.
CCM gives you the relationship and the structured touchpoints. RPM gives you the data that makes those conversations more meaningful. Instead of asking, “How have you been feeling?”—you’re saying, “I see your weight is up three pounds this week and your blood pressure spiked twice. Let’s talk about what’s going on.”
Patients are more compliant when they have a consistent point of contact. Clinicians make better decisions when they have context. And operationally, you’re not fragmenting outreach across multiple programs—you’re creating continuity.
The reimbursement structure supports this when both programs are clinically appropriate and well-coordinated. But the bigger benefit is better care and better outcomes, which ultimately supports everything else you’re trying to accomplish in value-based care.
Let’s be honest about what actually stops practices from succeeding with CCM and RPM:
Staffing. These programs need dedicated, clinically trained people. You can’t bolt this onto someone’s existing workload and expect it to work.
Patient engagement. Enrollment takes effort. Sustained participation takes even more. Not every patient will say yes, and not every enrolled patient will stay engaged.
Documentation and compliance. Medicare’s requirements are specific. Miss a detail, lose the revenue. There’s no margin for sloppiness.
Workflow integration. If CCM and RPM feel like add-ons rather than core functions, they’ll always struggle. They need to fit naturally into your EMR, your care team structure, and your clinical rhythm.
These are solvable problems, but they require commitment. The practices that treat CCM and RPM as strategic initiatives succeed. The ones that treat them like side projects don’t.
The 2026 rate increases aren’t just about more dollars per code—they’re a continuation of a clear trend. Medicare is rewarding practices that invest in proactive care for complex patients. That direction isn’t changing.
With higher reimbursement in place, this is a logical time to evaluate whether you’re positioned to capture it. Not because you need to rush, but because the foundational work—staffing, workflows, compliance processes—takes time to build properly.
Here’s what you need to ask yourself:
If you don’t have clear answers, 2026 is a reasonable year to develop them. The practices that address these questions now will be better positioned not just for today’s reimbursement, but for the continued evolution of care delivery beyond the traditional visit model.
The opportunity is here. Whether you’re ready to act on it is the question worth answering.